What is a macrophage?
Macrophage is a kind of white blood cell widely existing in blood source and tissue. It is a key component of innate immunity and plays an important role in human immune system. It has many functions such as phagocytosis and digestion of invading microorganisms. Remove cell debris and dead cells; And stimulate other cells involved in immune function.
Macrophages are derived from monocytes, which themselves are derived from bone marrow. Monocytes circulate in the blood for one to three days and then migrate into tissues, where they become macrophages or dendritic cells. Macrophages are found in many organs of the body, including the liver, brain, bones, and lungs, as well as in the blood, especially at the site of infection.
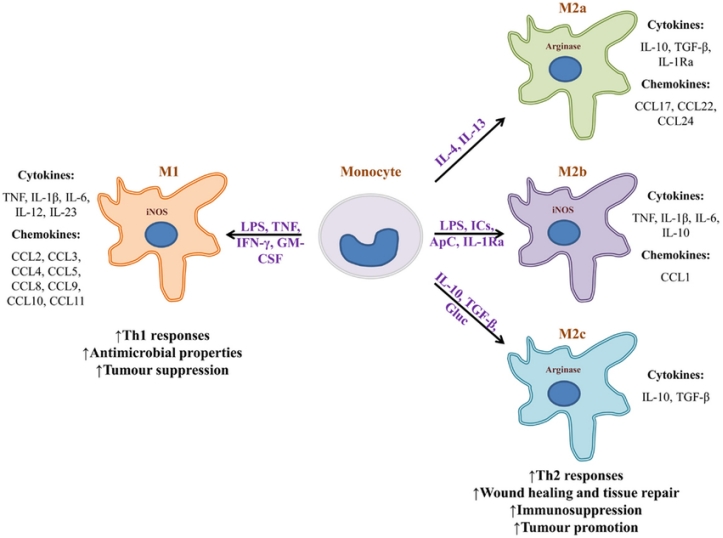
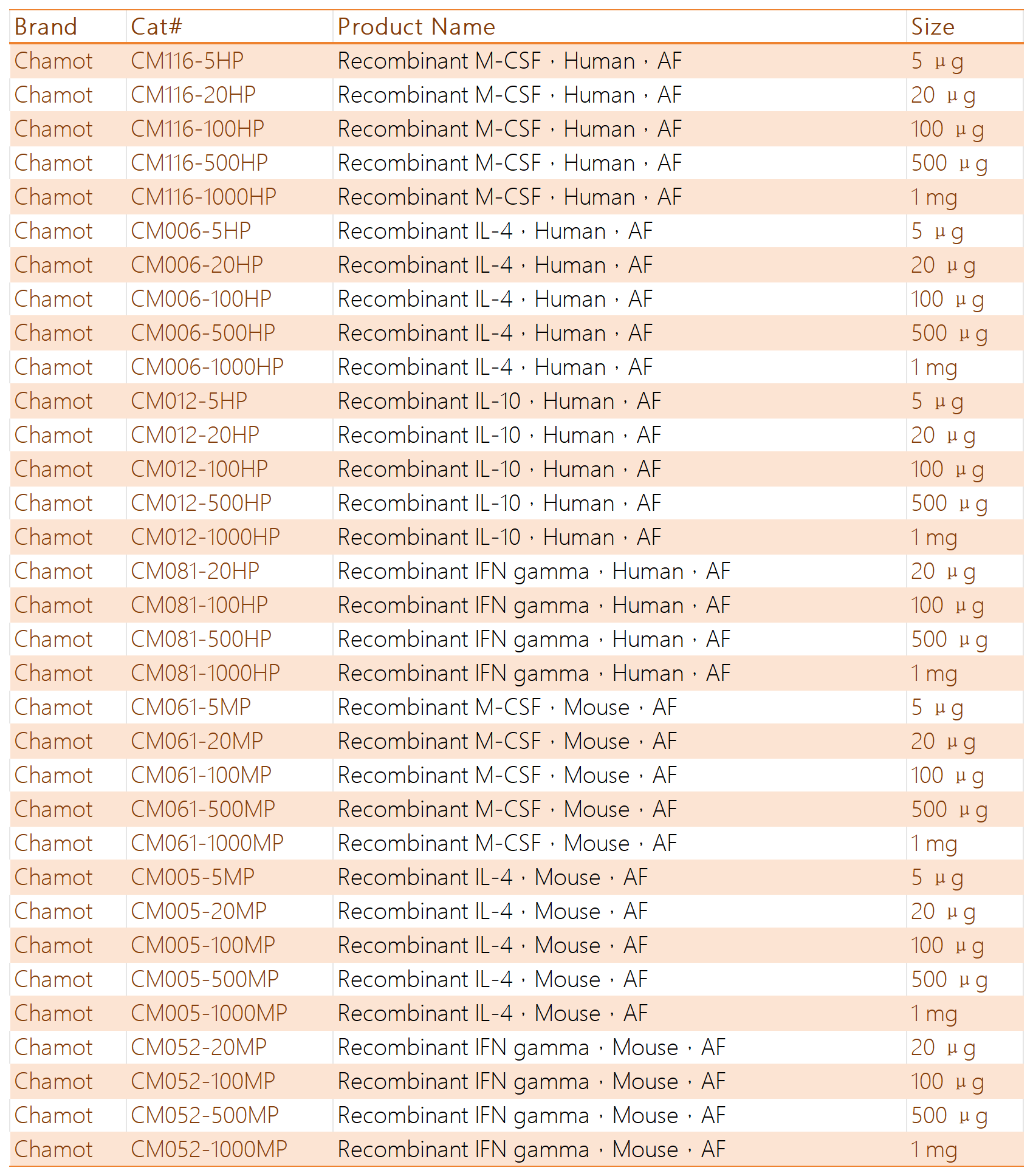
Fig.1 Monocytes can become phenotypically distinct macrophages( From:Guillermo Arango Duque, etc. Front Immunol. 2014 Oct 7;5:491.)
What are the types of macrophages?
Macrophages are classified into two types, and their phenotypes are: pro-inflammatory M1 phenotype and anti-inflammatory M2 phenotype. M1 macrophages release cytokines and chemokines, which are necessary for lymphocyte activation and recruitment to the site of inflammation. Macrophages also have antigen-presenting functions necessary to induce humoral immune responses. In addition, activated M2 macrophages control and address inflammation by releasing anti-inflammatory cytokines. These macrophages are involved in wound healing, tissue repair and remodeling after inflammation. M1 activity inhibits cell proliferation and promotes tissue damage, while M2 activity induces tissue regeneration and stimulates cell proliferation. Differences in functional properties of M1 and M2 macrophage subsets are reflected in differences in arginine metabolism. M1 macrophages have a unique ability to produce the "killer" molecule nitric oxide (NO) from arginine, which is widely used to damage and kill pathogens by producing peroxynitrite. In contrast, M2 macrophages convert arginine into the "repair" amino acid molecule ornithine, which is further involved in the synthesis of proline and polyamines.
In macrophages, polarization and phenotypic switching are accompanied by overall changes in the cell's transcriptome and proteome, which are tightly regulated by exogenous and intrinsic stimuli. Failure to control the plasticity of macrophages can lead to maladaptive reactions, leading to inflammatory diseases and tissue damage (in the case of excessive M1-polarization response) or tissue fibrosis and cancer (in the case of excessive M2-polarization response).
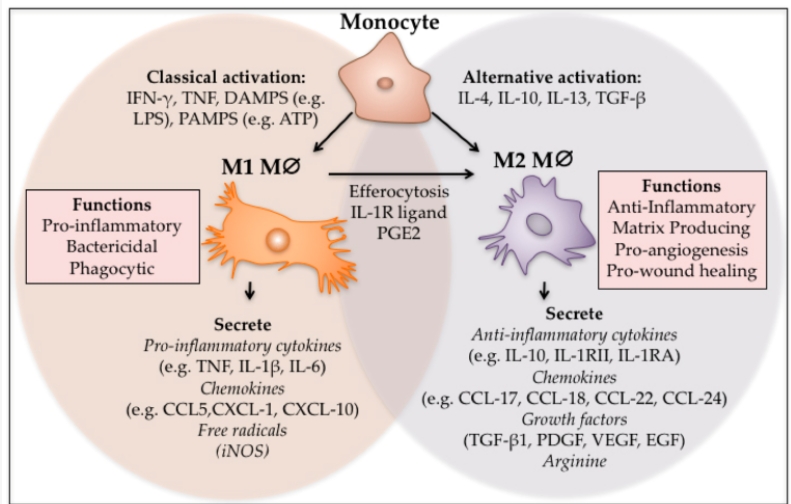
Fig. 2 M1 and M2 polarisation of macrophages.
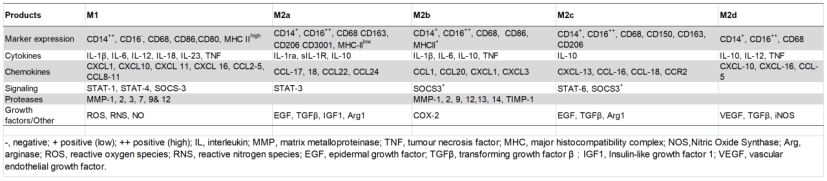
Fig.3 Human M1 and M2 phenotypes.(From: Mark Hesketh, etc. Int J Mol Sci. 2017 Jul 17;18(7):1545.)
Macrophages were cultured in vitro
In vitro studies of macrophage polarization, M1-type polarization is usually induced by TLR agonists such as GM-CSF or IFN-γ and LPS, and M2-type polarization is induced by M-CSF and Th cytokines such as IL-4, IL-13, and glucocorticoids, and then changes in gene expression, cell surface markers, and protein content and activity are detected. At present, there are three main types of human macrophages cultured in vitro, namely, mononuclear cells with infinite proliferation THP-1, primary isolated mononuclear cells such as MDM from PBMCs or BMDM from bone marrow.
| Cell | Medium | Initial Addition | M1 polarization | M2 polarization |
|---|---|---|---|---|
|
THP-1 |
RPMI 1640 |
100ng/ml PMA |
20ng/ml IFN-γ |
20ng/ml IL-4 |
|
PBMCs(MDM) |
RPMI 1640 |
50ng/mL G-CSF or |
10ng/ml LPS |
20ng/ml IL-4 |
|
BMDM |
IMDM |
10ng/ml M-CSF |
100ng/ml LPS(with 50 ng/ml IFN-γ) |
10ng/ml IL-4(with10 ng/ml IL-13) |
Relate Products